“There’s nothing about an Achilles rupture that should prevent him from coming back better than he was before.”
That was the message from Dr. Kevin R. Stone, an orthopedic surgeon at The Stone Clinic and a leading expert in Achilles tendon repair, in the immediate aftermath of Jayson Tatum’s injury.
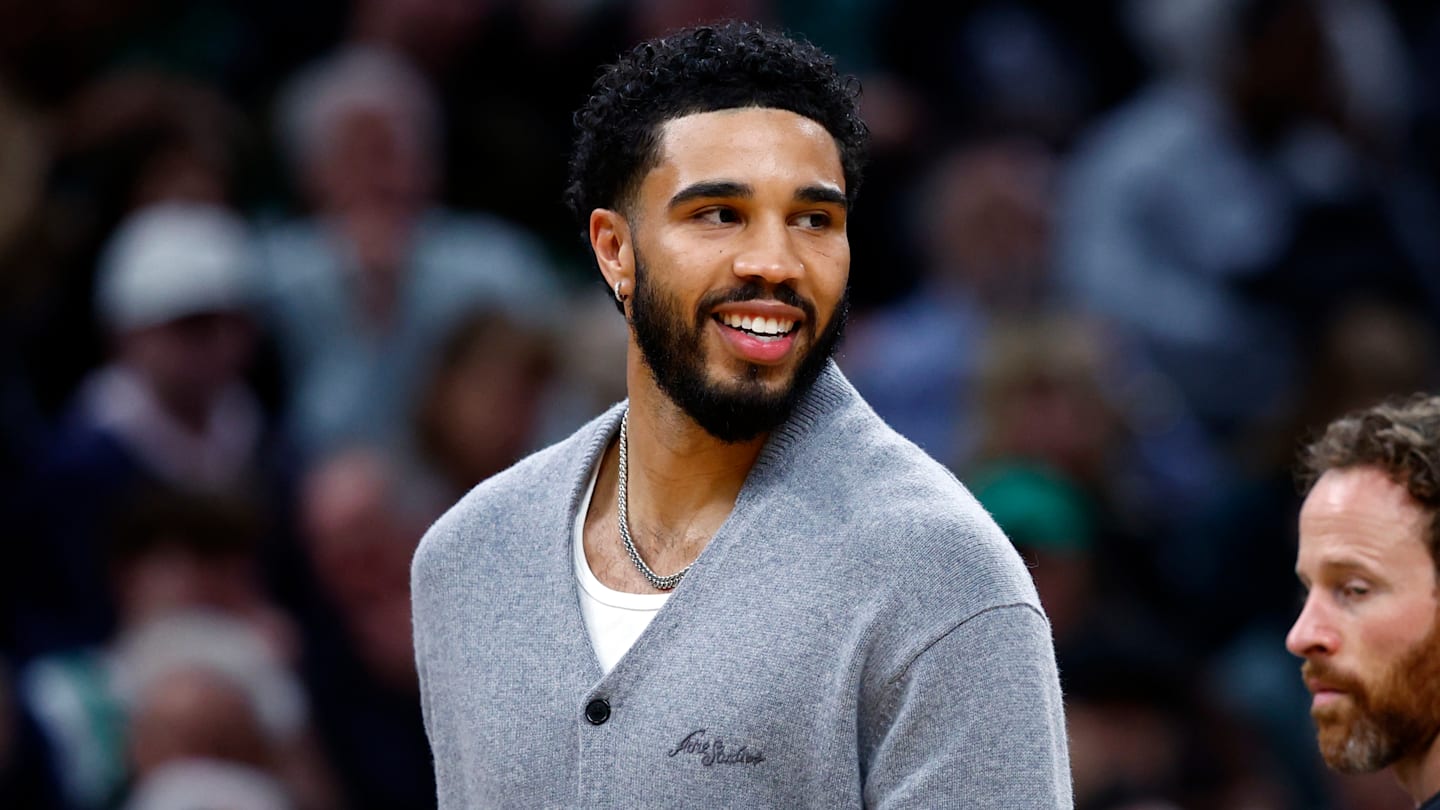
The time spent rehabbing is also a chance for the Boston Celtics star forward to learn more about his body and train parts that didn’t receive as much attention before an injury he vows won’t define him.
That’s an essential step in maximizing his time recovering and ultimately making Dr. Stone’s declaration a reality. It’s a box Tatum’s checking by relentlessly attacking his rehab.
“I’m feeling better, though, I’ve had 29 weeks to, like, really work on my body. This [is] the strongest I’ve ever been, the best the rest of my body has ever felt,” said Tatum during a recent appearance on The Morris Code, a podcast hosted by former NBA players Marcus and Markieff Morris.
What to know as Jayson Tatum’s return inches closer
His disciplined approach, including spending most of his summer at the Auerbach Center, the Celtics’ practice facility, has earned rave reviews from the organization.
He has now reached the point where he is playing one-on-one against members of the team’s coaching staff. With each encouraging update, the questions about when he will return grow louder.
That’s why Hardwood Houdini checked in with Dr. Stone for insight into what goes into assessing whether Tatum has fully recovered and what to know about his return to play.
Watching the six-time All-Star play one-on-one and go through on-court drills, one might wonder if the way he is attacking his rehab has him ahead of schedule.
“The reality is that we don’t actually know the strength of a well-heeled Achilles tendon at each time point after injury and repair,” shared Dr. Stone. “Clearly, we do know that as you apply force to collagen structures, the more force you apply in a gradual way, the stronger the collagen gets. And so in a great athlete like Jayson, who’s been applying a training regimen to his healing Achilles tendon, that tendon most likely is healing stronger than the average bear who might have just put it in a boot and not really trained.
“So, the likelihood is that his Achilles tendon is stronger than somebody else who didn’t train as hard. And the reality is, we don’t know how strong it is. The fortunate thing is that we rarely see repeat ruptures after a well-healed Achilles tendon that’s been repaired properly. And in our own studies of MRI of Achilles tendons, they all hypertrophy. They all look thicker after repair in the first few years. And it really does persist, actually, for a lifetime. We can tell a repaired Achilles tendon from one that wasn’t repaired. So we suspect that the restrictions on return to play have always been a little bit too conservative.”
As Tatum and the Celtics have repeatedly reiterated, the four-time All-NBA First Team selection must “check the boxes” along his road to recovery before he can rejoin the lineup.
But what boxes are the most significant ones for him to check off?
“There’s obviously the physical boxes: returning to your strength, returning to your jump height, returning to your flexibility,” said Dr. Stone. “But most importantly, there’s the mental return, meaning, can you get the fear of a rupture out of your head? And then, can you sprint and stop and launch and jump, and without that little nagging feeling that, ‘Oh, maybe I need to protect my Achilles.’
“And usually, that does go away pretty soon once you’ve been out on the court; once you’ve been back in the game. But it’s still a little nagging fear in the back of the mind.”
Jayson Tatum’s timeline to return
As the 27-year-old star forward works to get back to 100 percent and get the green light to return, those examining his Achilles tendon are looking for specific characteristics.
“Number one, the sports testing,” said Dr. Stone about what the medical experts evaluating Tatum’s Achilles tendon will want to see before clearing him. “Number two, repeat MRI. You can get a good assessment of the health of the Achilles tendon by a repeat MRI.
“Tendons that look nice and black on [an] MRI and thick and well-healed are generally good tendons. Tendons that have a lot of white streakiness in it sort of indicates that the healing process is not complete.”
Could an MRI of Tatum’s Achilles tendon reveal the desired results in time for him to return in January? Depending on the date he walks out onto the TD Garden parquet in a Celtics uniform for the first time, that would be roughly eight months after his injury.
“It’s definitely realistic,” Dr. Stone stated matter-of-factly.
Still, even if Tatum gets medically cleared, is it in his best interest and the franchise’s best interest long term to wait for him to return next season?
“No. The longer you’re out, the harder it is to come back,” conveyed Dr. Stone. “And that’s pretty much true in every sport. But it’s especially true after a significant injury, because it takes that injury fear pattern and stretches it out.
“Will I be as good? Will I be back? Is there a spot for me? Will my jump be as good? And the quicker you’re back on the horse, in a sense, the quicker you’re back in the game, in general, the faster you get over the injury and return to your sport. And again, our goal is to have him return better than he was before.
“So, one of the most important things an athlete does with an injury is they use the time to think through what did they not focus on before? What can they focus on now a little bit better? The core strength, upper body strength, balance, agility, things that you can train really while you’re recovering from the one injury that you’re relatively protecting. So, the hope is that you come back, not only a fitter, faster, stronger athlete, as we like to say, but a smarter one too.”
Jayson Tatum’s workload upon returning
Then, there’s the matter of how many minutes the St. Louis, Missouri native is playing per game. Can he log 20 consistently? Does it need to be fewer? Can he handle even more?
“Yes. It’s not a matter of the workload, it’s a matter of the strength of the tendon. So, if the tendon’s healed well, there’s no reason why you can’t increase the volume,” shared Dr. Stone.
Growth factors, such as platelet-rich plasma [PRP] injections, will aid in the healing process and help Tatum return to play faster than he would without them. It’s a significant part of the evolution of treating perhaps the most devastating injury in sports. It’s an advantage that even those who tore their Achilles tendon a few years ago likely didn’t have on their side.
“Another part of the story that we don’t know, because we don’t have the inside information about how much he has used growth factors such as PRP and therapies that are legal within the sport to augment the healing,” expressed Dr. Stone.
“But now, in almost every one of these injuries, in every ankle sprain, almost every soft tissue injury that we see, in order to help the athlete come back faster and stronger, we add these growth factors to these injuries. And so his Achilles tendon, assuming it was treated that way, is different than the Achilles tendons that ruptured a few years ago, where they didn’t receive that treatment.”
The science behind the most significant advantage of receiving those injections translates to being safer to return sooner.
“The injections are potently anabolic, meaning they stimulate collagen formation. They’re anti-inflammatory, meaning they bring down the inflammation around the injury. They’re anti-fibrotic, meaning they diminish the scar tissue formation. And most importantly, they recruit the body’s own stem cells to the site of [the] injury. And so all of us are sitting here with billions of stem cells in our body. And when you add these recruitment factors, you can increase their migration to the site of [the] injury and speed up their repair.”
Is it safe for Tatum to play in the postseason?
Minutes in the playoffs are more stressful on the body and the mind. The intensity increases, and the toll becomes more taxing. If Tatum doesn’t return until mid-March or later, should the Celtics hold him out in the playoffs?
“It really depends on him, the training, the fitness, the testing, the MRI, a whole host of factors would go into it,” said Dr. Stone. “In general, if the tendon’s well healed on fitness testing and MRI, there’s no reason why he can’t return fully.”
And just as the athletes before Tatum who tested the limits of what they could do after tearing their Achilles tendon paved the way for the advancements that are aiding the Celtics’ star’s hopes of returning even better, how he’s attacking his rehab and what happens when he takes the court again will benefit those who go through this injury after him.
“We always learn the most from our patients who cheat,” voiced Dr. Stone. “By cheating, I mean that they don’t listen to our advice. They throw away the crutches earlier than we thought. They come back in and teach us that our guidance may have been too conservative and too slow for them.
“And so we, in the sports medicine side of this world, have learned so much from our athletes who’ve really pushed the limits; taken our advice, but didn’t follow it to a T. And we learned from them about what’s possible. So I’m sure that every other top-level athlete who ruptures his Achilles this year will come to physicians like me for a percutaneous repair and then augmentation with growth factors, because the old methods of open surgery and not augmentation just take too long to heal from, and so his example will be a great example of top-level care augmented by biology.”